Migraine
Introduction by Esther Lardreau-Cotelle |
 January 2008 |
| Translation by Karine DEBBASCH |
|
Terminological remarks
The major nineteenth-century encyclopedias digitized on Medica feature articles on "cephalea", "cephalalgia", "migraine", "hemicrania", "head pain" or "carebaria" (literally, "head weightiness", "head heaviness"). But the entries are sometimes separated, or on the contrary joined together, and some articles are sometimes altogether absent: the Dictionnaire de médecine et de chirurgie pratiques for instance (articles on "cephalalgia"Migraine, hemicrania, cephalea, cephalalgia, head pain, head illness, etc.: a large number of terms, whose different meanings are not self-evident, refer to what is commonly called "headache".
Etymology, in this particular case, is of little help.Migraine and hemicrania are alterations from the Medieval Latin: via the Late Latin word hemicrania, or hemicranium, which apparently was more frequently used, hemigranea, hemigrania, migranea and migrana were borrowed from the Greek hemicranion and hemicrania, themselves composed of hemisus (half) and cranion (cranium). These terms refer to half the head as the locus of the migraine (hemicrania) and also to the pain felt in this half of the head: the illness coincides with its anatomical localization. In Greek or Latin Antiquity, it was indeed quite frequent to name a disease after the affected locus, so that analyzing the names of the diseases often amounts to defining them.
Although migraine and hemicrania are, from an etymological point of view, perfect synonyms, the two words are not used with the same meaning. As for any doublet, or any pair of words issued from the same etymon, each word acquired one particular meaning. The common word ‘migraine’ appeared in the 12th century with the non-medical acception of "despite, boredom" (this meaning survived until the late 19th century, for instance through the verb "migrainer" ("to migraine") [1]: "to cause a migraine, aggravate considerably, bore", which one can notably find in the Goncourt brothers’ writings); it had a normal phonetic evolution and underwent quite important modifications of its meaning in the course of two centuries. The more learned "hemicrania", on the contrary, seems to have appeared in the 16th century (Ambroise Paré used the word), at the time of the re-Latinization of the French language; directly borrowed from the Latin and the Greek, it only underwent minor transformations. Due to this phonetic evolution, migraine is, in its form, further away from the etymon, and it also presents a looser connection between signifier and signified than the word hemicrania does.These two terms should therefore not be considered as exact synonyms. Between the 16th and the 20th centuries, ‘hemicrania’ was used to refer to unilateral headache, whereas the word ‘migraine’, its etymology forgotten, was used – as early as the end of the 18th century (by Tissot, for example), but mostly during the 19th century – to refer to extremely varied forms, from forms accompanied by bilateral pain to painless ones.
Until a date that can be situated between 1829 (Prosper Martin) and 1831 (Pierre-Adolphe Piorry), the term ‘hemicrania’ was systematically chosen over ‘migraine’ [2]. But afterwards, ‘migraine’ prevailed, and hemicrania became used only to refer to a symptom. Migraine was no longer a mere anatomic definition, and the tendency was, on the contrary, to emphasize a series of symptoms and prodromes that so far had not been neglected altogether, but considered as very secondary when compared to the defining sensation of pain. 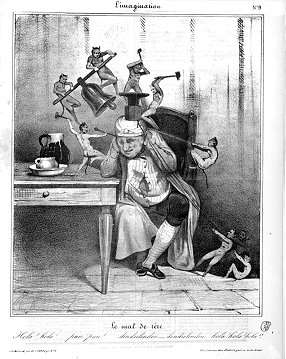 |
|
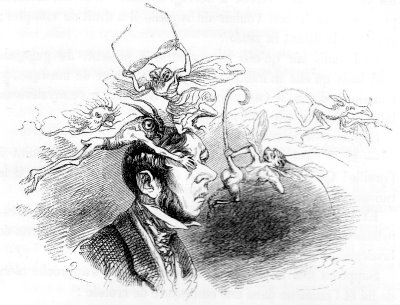
Honoré Daumier. Le mal de tête (The Headache) |
 |
|
Vapors. - Album comique de pathologie pittoresque, |
Rejection of the concept of pain
Most of the texts that are digitized here date from the 19th century, which is particularly rich in academic publications on migrainous diseases – medical students’ dissertations, monographs, dictionary articles, articles from periodicals, chapters from textbooks or courses – but also novels [4], vaudevilles [5], operettas [6], lithographs [7], etc.The decision to digitize documents was not accidental. Some texts, either because the Bibliothèque Interuniversitaire de Médecine does not possess them or because there are beneficiaries, could not be digitized – which is why some important references in the history of migraine are not available for on-line consultation, although they are featured in the bibliography.
But the corpus has also been deliberately restricted, at least in part, to the late 18th and the 19th centuries, insofar as the concept of migraine fully developed during that particular period of time. It would be wrong and anachronistic to believe that "migraine has always existed." A given medical problem appears at a given time, in a given place, according to a particular state of medicine and physiology or pharmacology. Nevertheless, the sensations of migraine and the facts of the disease probably are perennial.Diseases are to be viewed in their cultural environments. Particular time periods or regions tend to elect one disease as representative of their history. Each period, each country, has its "own" diseases. In the 18th century, the French often referred to the pox as "the Neapolitan disease", which the English called "the French sickness". England suffered from the spleen. Nineteenth-century France had "migraine": "one may say that France is the homeland of migraine" [8]. For nineteenth-century France, after the Revolution and the Terror, migraine was a real problem, and was a grimacing image of the various fractures in the country, be they social or sexual. It was the disease of intellectuals, the disease of ill-married women, the disease of the bourgeoisie.
It would nevertheless be wrong to believe that in ancient times "head pain" was an unknown disease. It would also be wrong to think that people in the 19th century refused to look back on previous centuries.
On the contrary, 19th-century medical dissertations were
all supposed to feature a summary of the knowledge acquired in the
course of Antiquity. The writings of Galen
![]()
![]() , Pseudo-Galen
, Pseudo-Galen
![]()
![]() , Aretaeus
, Aretaeus
![]()
![]() , Caelius Aurelianus
, Caelius Aurelianus
![]() or Alexander of Tralles
or Alexander of Tralles
![]() were seldom read (the references often were second hand), but
they kept being repeated. As for the Hippocratic corpus, it was only
mentioned to provide authority; indeed, although it does contain
words such as "cephalalgia", "head pains",
"pains around the head", "heaviness in the
temples", "heaviness in the head", there is nothing in
it that portrays the migrainous disease – apart from a passage from Epidemics
were seldom read (the references often were second hand), but
they kept being repeated. As for the Hippocratic corpus, it was only
mentioned to provide authority; indeed, although it does contain
words such as "cephalalgia", "head pains",
"pains around the head", "heaviness in the
temples", "heaviness in the head", there is nothing in
it that portrays the migrainous disease – apart from a passage from Epidemics
![]()
![]() , which seems to describe ophthalmic migraine, without
attributing it explicitly to migraine.
, which seems to describe ophthalmic migraine, without
attributing it explicitly to migraine.
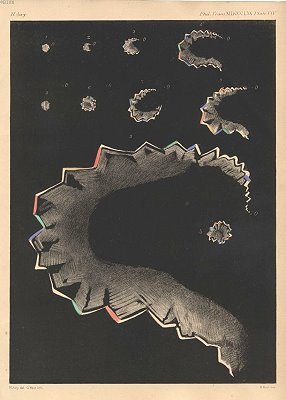
For quite a few years, parallel traditions, namely veterinary medicine and astronomy, had actually been shedding light on "strange" ocular phenomena – hemiopsy [9], phosphenes [10], etc. – followed by cephalalgia; the medical tradition, starting with Hippocrates, had considered these as part of a specific disease, scotodynia [11]. Medicine therefore considered it impossible to separate these phenomena from migraine.
Fothergill’s is one of the first medical texts to mention ophthalmic aura, that series of ophthalmic symptoms that are generally experienced at the onset of or just prior to a migraine headache; his work nevertheless was not known before Hubert Airy and Liveing
But the founding dissertation, thanks at once to its impact and to
its decisiveness, is that of Piorry, who invented the concept of
ophthalmic migraine [12] (see also Jules Pelletan de Kinkelin
![]() ): among the various sensations a patient is likely to
experience, ophthalmic symptoms (in particular scintillating scotoma
[13]), close to vertigo (Mémoire sur le vertige
): among the various sensations a patient is likely to
experience, ophthalmic symptoms (in particular scintillating scotoma
[13]), close to vertigo (Mémoire sur le vertige
![]() ; see also Ménière’s article
; see also Ménière’s article
![]() ), or speech deficiencies, are no less decisive than the
pain itself. Piorry’s work was furthered by Liveing’s book and
Hubert Airy’s article, previously mentioned, and also by three
important medical dissertations: that of Dianoux
), or speech deficiencies, are no less decisive than the
pain itself. Piorry’s work was furthered by Liveing’s book and
Hubert Airy’s article, previously mentioned, and also by three
important medical dissertations: that of Dianoux
![]() , who presented what physicians knew about the condition
in 1875; that of Robiolis
, who presented what physicians knew about the condition
in 1875; that of Robiolis
![]() who, in 1884, investigated the hypothesis of the
ophthalmologist Nicati (who had envisaged "migraines" for
each special sense organ (i.e. ophthalmic, auditory,
olfactory and gustative migraines); and that of Fink
who, in 1884, investigated the hypothesis of the
ophthalmologist Nicati (who had envisaged "migraines" for
each special sense organ (i.e. ophthalmic, auditory,
olfactory and gustative migraines); and that of Fink
![]() , in 1891, who presented what was known at the time on
hysterical migraine. The three decisive articles by Galezowski
, in 1891, who presented what was known at the time on
hysterical migraine. The three decisive articles by Galezowski
![]()
![]() , Féré
, Féré
![]() and Babinski
and Babinski
![]() were also a continuation of Piorry’s work.
were also a continuation of Piorry’s work.
|
Depiction of scotomas. - Hubert Airy, |
The old definition of "migraine" then appeared as inadequate: not only had the history of medicine shed light on hemicranias that were not migraines, but there seemed to be migraines that presented other types of symptoms than pain (Labarraque
The point nevertheless was not to replace the old definition with another one, equally nominal, but to substitute clinical descriptions for that definition.
For physicians as different from one another as Trousseau and Liveing, the starting point was no longer in a theoretical definition, but in what could be observed, be it a) at the hospital or b) in the laboratory (experimentation).
a) One cannot but notice that a number of cases reported in the
medical literature come from hospital or asylum populations [14].
Connections can therefore be made between patients who do not
belong to the same nosographic groups [15]. The family history of
the patient (his or her heredity), his or her personal history,
and the efficacy of a given antimigrainous treatment are essential
for the diagnosis: phenomena different from those that migraine
usually features are not a priori excluded, provided they
belong to a migrainous history, and can be treated with
antimigrainous drugs. Links might therefore be made between
diseases as seemingly different from one another as gout and
migraine (Trousseau, Chaumier
![]() , Soula
, Soula
![]() ), epilepsy and migraine (Liveing, all the texts by
Féré presented here, Gowers), or hysteria and migraine (Babinski,
Fink) – transformations, or similitudes. Room is made for
marginal, irregular forms, as well as for minimal and attenuated
forms of the disease which, were it not for the history of the
patient and the history of his/her family, would fail to be
recognizable: yawning, episodes of muteness, itching, congestion
of the face, vertigo, formation of bright images on the retina,
can all fall under a migraine diagnosis.
), epilepsy and migraine (Liveing, all the texts by
Féré presented here, Gowers), or hysteria and migraine (Babinski,
Fink) – transformations, or similitudes. Room is made for
marginal, irregular forms, as well as for minimal and attenuated
forms of the disease which, were it not for the history of the
patient and the history of his/her family, would fail to be
recognizable: yawning, episodes of muteness, itching, congestion
of the face, vertigo, formation of bright images on the retina,
can all fall under a migraine diagnosis.
- either two contradictory models of migraine (Du Bois-Reymond, Möllendorff);
- or two types of migraine, vasoconstriction migraines on the one hand (commonly called "white migraines", or scientifically "sympatheticotonic migraines"), and vasodilation migraines on the other ("red migraines", or "neuroparalytical migraines") (Eulenburg);
- or else, two different moments in a migraine crisis: an initial phase of vasoconstriction, followed with a phase of vasodilation (Latham, Jaccoud).
This change in perspectives did not deter researchers from working
on forms of migraine in which pain was prevalent. An extremely
rare form was thus isolated: ophthalmoplegic migraine [18] (also
referred to as "Möbius’ disease
![]() ", or as "Charcot-Möbius’ syndrome"), a
migraine accompanied by paralysis of some eye muscles (from the
Greek ophtalmos: eye, and plege: blow). Charcot
", or as "Charcot-Möbius’ syndrome"), a
migraine accompanied by paralysis of some eye muscles (from the
Greek ophtalmos: eye, and plege: blow). Charcot
![]() may not have been the first to describe it (in 1860,
Gubler
may not have been the first to describe it (in 1860,
Gubler
![]() described a paralysis of the stem of the oculomotor nerve,
preceded by migraines, although it is not entirely clear that one
can consider it as a real "ophthalmoplegic migraine".
Nevertheless, in 1890 Charcot gave it the name under which it has
been known ever since.
described a paralysis of the stem of the oculomotor nerve,
preceded by migraines, although it is not entirely clear that one
can consider it as a real "ophthalmoplegic migraine".
Nevertheless, in 1890 Charcot gave it the name under which it has
been known ever since.
Other texts, some of them published in the first half of the 20th century, are just as important as the ones mentioned above. Wolff and his colleagues rekindled work on the vascular hypothesis [19]. As for the neurological hypothesis [20], it was considerably enriched by a series of articles by Lashley [21], Leão [22], and Milner [23].
Treatments
It is commonly thought that therapies in the past were inconsistent, and were nothing but a mix of ill-conceived procedures, resulting more from a vague "magical" thinking than from rational thinking.But this opinion cannot be maintained in view of the documents we have. The medications proposed during a given period were indeed consistent with the theories of that period, even though one may occasionally notice some discrepancies.
It is impossible to summarize in just a few lines the whole range of pre-19th-century therapies, as they varied both according to the schools and according to the type of head pain one wished to treat. The treatments usually promoted, as a general prevention, [24] both a dieting and a healthy lifestyle: practicing gymnastics, bathing, walking, traveling, playing games for the spirit and/or for the body [25] were recommended to avoid feeling unhappy, bored, angry or worried, but also to avoid an excess of feelings. The purpose of the diet was to facilitate digestion and to avoid plethora, one of the major causes of hemicrania.A few categories of medications based on different principles can nevertheless be listed.
- 1°) The "cephalic remedies" (verbena, ambergris, camphor, orange flower water, etc.), the use of which was to disappear, were recommended against "head pains", not only against hemicrania. These remedies were supposed to play some obscure role on the brain, the nerves and their diseases, improving one’s understanding and memory, curing epilepsy, manias, paralysis, pains, imbecility, etc.
- 2°) Other specifics, the "anodyne remedies" (mullein flower, elder flower, poppy, linden, etc.), were taken to anaesthetize pain.
- 3°) The purpose of some therapies was, on the contrary, either to provoke a new, stronger pain in some other part of the body, or to somehow stimulate a part of the body to create a diversion. This was achieved by moxibustion, ustion, or by vesicatories (creating blisters on the skin) – which, by causing a second, artificial point of irritation, counterbalanced the pain felt in another area. Cauteries were used to awaken the sensitivity. The technique of frictions had the same purpose, as observed by Roselyne Rey [26].
- 4°) Based upon the humoral theories, purgation or emesis, bloodletting, arteriotomy, suction cups or leeches, and sternutation were used in order to evacuate humors. Some substances were also administered in the treatment of head pains for their complementary properties; it was the case of hellebore, which acts both as a drastic purgative and as a narcotic.
- 5°) Physicians sometimes chose to promote maturation or suppuration of the pain: these were among the roles of ointments and plasters.
In the 19th century, the specifics (cephalic and anodyne remedies) disappeared. The violent criticism of polypharmacy (pharmacy based on the massive and multiple prescriptions of medicinal substances) was approximately contemporary with the criticism of the concepts of "head disease" and "head pain". The therapies varied along with the theoretical models of migraine.
- 1°) The analogy with epilepsy made some prescribers use potassium
bromide [27]. In 1867, Barudel, a military doctor [28], was the
first one to use it in the treatment of migraine, while some ten
years earlier Charles Locock had used it against hystero-epilepsy
and in 1858-1859, Wilks and Radcliffe had used it in cases of
epilepsy. Charcot
 systematized its recourse against migraine as – in his words
– an empirical and analogical, but successful treatment.
systematized its recourse against migraine as – in his words
– an empirical and analogical, but successful treatment.
- 2°) Bromide was however ineffective against hysterical migraine, and a hypnotic therapy was prescribed in such cases.
- 3°) Against migraine as a manifestation of gout or rheumatisms,
physicians used medications known to be efficacious against these
diseases: colchicum, sodium bicarbonate, hydrotherapeutic cures [29]
[30], salicylates
 or pyrazolates
or pyrazolates
 .
.
- 4°) And finally, against the vascular forms of migraine, either vasoconstrictors or vasodilators were used, depending on the type of migraine; in angio-paralytic forms, with vasodilation, rye ergot was prescribed; in sympathetico-tonic forms, with vasoconstriction, amyl nitrite and chloral (chloral hydrate) were favored.
The faradaic current, an alternative current obtained by induction with a variable magnetic field (Ruhmkorff or Clarke coils), produced discontinuous rhythmic muscular contractions (a significant interval separated the end of one wave from the beginning of the next one) that were used to increase blood flow and diminish muscle inflammation.
Prior to 1870, small portable devices were manufactured, allowing doctors to take to their patients’ homes a cell that was powerful enough| Faradization | Galvanization | Mixed apparatus | |||
 
|

|
 |
 |
||
|
Faradization Galvanization Mixed
apparatus |
DC electromagnetic
apparatus, for galvanization. Made by Ch. Chardin in Paris, ca.1875. © Private collection, ASPAD |
Mixed electromagnetic apparatus |
|||
More generally, the history of pharmacy underwent a second transition at the end of the 19th century: the appearance of medication packaging implied a new relationship between migraine sufferers on the one hand and physicians and pharmacists on the other. Physicians themselves started advising their patients to keep powders and tablets on their persons, even though they were aware that this came down to delegating a part of their power. Medical advertising had been forbidden in France until 1867 for fear of quackery; the near monopoly of Bayer and the arrival of synthesized products issued from German research (notably antipyrin) changed migraine into a commercial object
Bibliographical elements
Summary indications. Primary sources
Secondary sources
| Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders, 2nd edn. Cephalalgia 2004, vol. 24 (Suppl. 1) : p. 27–8. |
| BRUNE (Kay). The early history of non-opioid analgesics, Acute Pain, décembre 1997, vol. 1, n° 1, p. 33-40 |
| CASS (Stephen P.), ANKERSTJERNE (Jennifer K. P.), YETISER (Sertac), FURMAN (Joseph M.), BALABAN (Carey), AYDOGAN (Barlas). Migraine-related vestibulopathy, Annals of Otology, Rhinology and Laryngology, 1997, vol. 106, p. 182-189 [BIUM Call Number 132.138] |
| GRANELLA (Franco), D’ANDREA (Giovanni). Hemicrania horologica (« Clock-like hemicrania »), Neurology, 2003, vol. 60, n° 10, p. 1722-1723 [BIUM Call Number 114.181] |
| HAUT (Sheryl). Differentiating migraine from epilepsy, Advanced studies in medicine, juin 2005, vol. 5 (6 E), S658-S665 |
| ISLER (Hansruedi). Episodic cluster headache from a textbook of 1745 : van Swieten’s classic description, Cephalalgia, juin 1993, vol. 13, n° 3, p. 172-174 [BIUM Call Number 96.879] |
| KOEHLER (Peter J.). Brown-Séquard’s comment on Du-Bois-Reymonds’ "hemikrania sympathicotonica", Cephalalgia, octobre 1995, vol. 15, n° 5, p. 370-372 [BIUM Call Number 96.879] |
| KOEHLER (Peter J.), ISLER (Hansruedi). The early use of ergotamine in migraine. Edward Woakes’report of 1868, its theoretical and practical background and its international reception, Cephalalgia, octobre 2002, vol. 22, n° 8, p. 686-691 [BIUM Call Number 96.879] |
| LARDREAU (Esther). The difference between epileptic auras and migrainous auras in the 19th century, Cephalalgia, 2007, vol. 27, p. 1378-1385. |
| LI (Bu K.), MURRAY (Robert D.), HEITLINGER (Leo A.), ROBBINS (Jennifer L.), HAYES (John R.). Is cyclic vomiting related to migraine? The Journal of Pediatrics, 1999, vol. 134, n° 5, p. 567-572 [BIUM Call Number 112.819] |
| LUCAS (Christian), GÉRAUD (Gilles), VALADE (Dominique), CHAUTARD (Marie-Hélène), LANTERI-MINET (Michel). Recognition and therapeutic management of migraine in 2004, in France : results of FRAMIG3, a french nationwide population based survey, Headache, 2006, vol. 46, p. 715-725 [BIUM Call Number 115.521] |
| McINTYRE (Roger S.), ZONARSKI (Jakub Z.), WILKINS (Kathryn), BOUFFARD (Beverley), SOCZINSKA (Joanna K.), KENNEDY (Sidney H.). The prevalence and impact of migraine headache in bipolar disorder : results from the Canadian community health survey, Headache, 2006, vol. 46, p. 973-982 [BIUM Call Number 115.521] |
| NEUHAUSER (Hannelore), LEOPOLD (Michael), BREVERN (Michael von), ARNOLD (G.), LEMPERT (Thomas). The interrelations of migraine, vertigo and migrainous vertigo, Neurology, 2001, vol. 56, p. 436-441 [BIUM Call Number 114.181] |
| PEARCE (John M.). Latham and the vasomotor theory of migraine, Seminars in neurology, 2006, vol. 26, p. 271-276 [BIUM Call Number 115.874] |
| PODOLL (Klaus), NICOLA (Ubaldo). L’arte emicrania come strumento di studio dell’ispirazione artistica, Confinia cephalalgica, 2001, n° 10, p. 137-144 |
| POST (Robert M.). Do the epilepsies, pain syndromes, and affective disorders share common kindling-like mechanisms? Epilepsy Research, 2002, vol. 50, p. 203-219 [BIUM Call Number 115.889] |
| POST (Robert M.), SILBERSTEIN (Stephen D.). Shared mechanisms in affective illness, epilepsy and migraine, Neurology, 1994, vol. 44, suppl. 7, S37-S47 [BIUM Call Number 114.181 suppl.] |
| REY (Roselyne). Histoire de la douleur (1993), Paris, La Découverte et Syros, 2000 [BIUM Call Number 351.542] |
| ROBINS (Lawrence), LUDMER (C.). Headache : the bipolar spectrum in migraine patients, Journal of Pain, 2000, vol. 10, p. 167-170 |
| RUSSELL (Michael Bjørn), OLESEN (Jes). A nosographic analysis of the migraine aura in a general population, Brain, 1996, vol. 119, p. 355-361 [BIUM Call Number 91.082] |
| SACKS (Oliver). Migraine. Understanding a common disorder, University of California Press (1985), Paris, Seuil, traduction française de Christian Cler, 1996 [BIUM Call Number 183.539] |
| SYMON (David N.K.). Is cyclical vomiting an abdominal form of migraine in children? Digestive Diseases and Sciences, 1999, vol. 44, n° 8, p. 23 S (p. 23 S – p. 25 S) [BIUM Call Number 113.169 Sup.] |
| YOUNG (W.B.), SIOW (H.C.), SILBERSTEIN (Stephen). Anticonvulsivants in migraine, Current pain headache reports, 2004, vol. 8, n° 3, p. 244-250 |